Bedsores, also known as pressure ulcers, and pressure injuries, are injuries that result from prolonged pressure on the skin, causing damage to the skin and underlying tissue.
(Source: myhealth.alberta.ca)
The healing process can vary significantly based on multiple factors, including the stage of the bedsore, the patient's overall health, the quality of care received, and the presence of any infections.
This article explores these factors in detail to provide a comprehensive understanding of how long bedsores take to heal. Always consult a trained physician when working through complications of pressure injuries to maximize your success in mitigating the issue.
Factors Influencing Healing Time
Stage of the Bedsore:
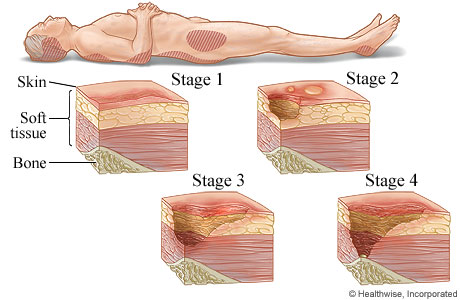
Stage 1: This is the mildest stage of a bedsore, characterized by red or discolored skin that does not break open. With proper care, such as relieving pressure on the affected area and keeping the skin clean and dry, Stage 1 bedsores can heal within a few days to a couple of weeks. Early detection and intervention are crucial for quick recovery.
Stage 2: At this stage, the skin breaks open, creating a shallow wound or blister. Healing Stage 2 bedsores can take several weeks to months. Treatment involves cleaning the wound, protecting it with appropriate dressings, and addressing any underlying health issues that may impede healing, including determining the cause of the wound as original.
Stage 3: These ulcers penetrate deeper into the skin, reaching the fat layer. Healing Stage 3 bedsores can take one to four months, depending on the individual's health and the care provided. Effective management includes debridement (removal of dead tissue), advanced wound dressings, and possibly the use of specialized beds or mattresses to reduce pressure, and increase movement.
Stage 4: This is the most severe stage, with extensive damage to the skin, muscle, and possibly bone. Healing Stage 4 bedsores can take several months to years. Treatment often involves surgical intervention to remove necrotic tissue and promote healing, along with intensive wound care and infection control measures.
Patient’s Overall Health:
The patient's overall health significantly affects the healing process. Chronic conditions such as diabetes, vascular diseases, and malnutrition can slow healing. For instance, diabetes can impair blood circulation and immune response, making it harder for the body to repair damaged tissue. Good nutrition, proper hydration, and managing underlying health conditions are vital for promoting faster healing.
Quality of Care:
Quality care is essential for the healing of bedsores. Proper wound care, which includes regular cleaning and dressing changes, helps prevent infection and promotes a healthy healing environment. Advanced therapies, such as negative pressure wound therapy (NPWT) and the use of pressure-relieving beds and mattresses, can enhance the healing process. Consistent and diligent care by healthcare professionals and caregivers can significantly reduce healing time.
Infection Prevention:
Infections can severely delay the healing of bedsores and lead to further complications. Preventing infections involves maintaining a clean wound environment, using appropriate antiseptics, and administering antibiotics when necessary. Early detection and treatment of infections are crucial to avoid prolonged healing times and additional health risks.
Management and Treatment
Nonsurgical Treatments:
Nonsurgical treatments are often the first line of defense against bedsores. These include cleaning the wound with saline or antiseptic solutions, applying moisture-retentive dressings, and using topical antibiotics to prevent or treat infections. Regular repositioning of patients to reduce pressure on vulnerable areas is also critical. Additionally, nutritional support, such as protein supplements, can aid in tissue repair and overall recovery.
Surgical Treatments:
In severe cases, surgical treatments may be necessary. Surgical options include debridement to remove dead tissue, skin grafts to cover large wounds, and flap surgery to close wounds with nearby tissue. Surgery is typically considered for Stage 3 and Stage 4 ulcers to expedite healing and reduce the risk of complications. Post-surgical care is essential to ensure proper healing and prevent recurrence.
Learn more about prevention of bedsores and pressure injuries with our helpful awareness guide on prevention methods.
Prevention and Outlook
Preventing bedsores is better than treating them. Preventive measures include regularly repositioning patients, maintaining skin hygiene, using pressure-relieving devices like specialized medical beds that provide automated patient rotation to shift and relieve pressure frequently, and ensuring adequate nutrition and hydration. Education of caregivers and healthcare providers about early detection and intervention strategies is also crucial.

Early intervention and consistent care can significantly improve the prognosis of bedsores. While early-stage bedsores can heal relatively quickly, advanced stages require prolonged treatment and may lead to complications if not managed properly. Comprehensive care that addresses all aspects of the patient's health and well-being is essential for optimal healing outcomes.
For more detailed information on bedsores and their treatment, visit the Cleveland Clinic's page on Bedsores.

